Around one million Americans may develop some form of dementia every year by 2060, according to a study published on Monday in Nature Medicine. The latest forecast suggests a massive and harrowing increase from annual cases predicted for 2020, in which approximately 514,000 adults in the U.S. were estimated to be diagnosed with dementia—an umbrella term that describes several neurological conditions that affect memory and cognition.
The new study also showed the lifetime risk of dementia increased progressively with older age. They estimated that after age 55, the lifetime risk of dementia is 42 percent, and continues to rise sharply to 56 percent after age 85. Groups that showed greater lifetime risks (between 44 and 59 percent after age 55) were Black adults, women and people who carried the allele APOE e4: this variation of the gene APOE, which codes for the protein apolipoprotein E, increases the risk of developing Alzheimer’s disease. Alzheimer’s is the most common cause of dementia, but the study focused on all forms.
“I knew the total lifetime risk would be higher than previous 20-year-old estimates,” says Josef Coresh, senior author of the study and founding director of the Optimal Aging Institute at the NYU Grossman School of Medicine. “But I didn’t expect that it would land at 42 percent.”
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Coresh’s team collected medical records from 15,043 people who had enrolled in the Atherosclerosis Risk in Communities Study (ARIC), a separate longitudinal study that has been investigating the connections between heart disease and cognitive health. The study cohort included adults between 45 to 64 years of age who did not have dementia at the time they were recruited. Approximately 31 percent of them were confirmed APOE e4 carriers.
Most medical experts define dementia as a collection of symptoms—such as life-impairing loss of memory, language and other cognitive functions—that stem from the degradation of brain cells. Coresh says a panel of medical experts evaluated participants’ symptoms and clinical data to make a dementia diagnosis. Dementia studies often rely on medical and death records, as well as on-site neuropsychological testing that measures a person’s mental state and detects signs of cognitive impairment. Coresh explains that people can forget scheduled visits when their cognitive health declines, however. ARIC investigators performed comprehensive risk assessments of each participant. And for those who missed in-person visits, they checked in annually or semi-annually by conducting telephone interviews with those individuals or “informants” such as relatives. The investigators corroborated dementia diagnoses in hospital or death records with informants whenever possible.
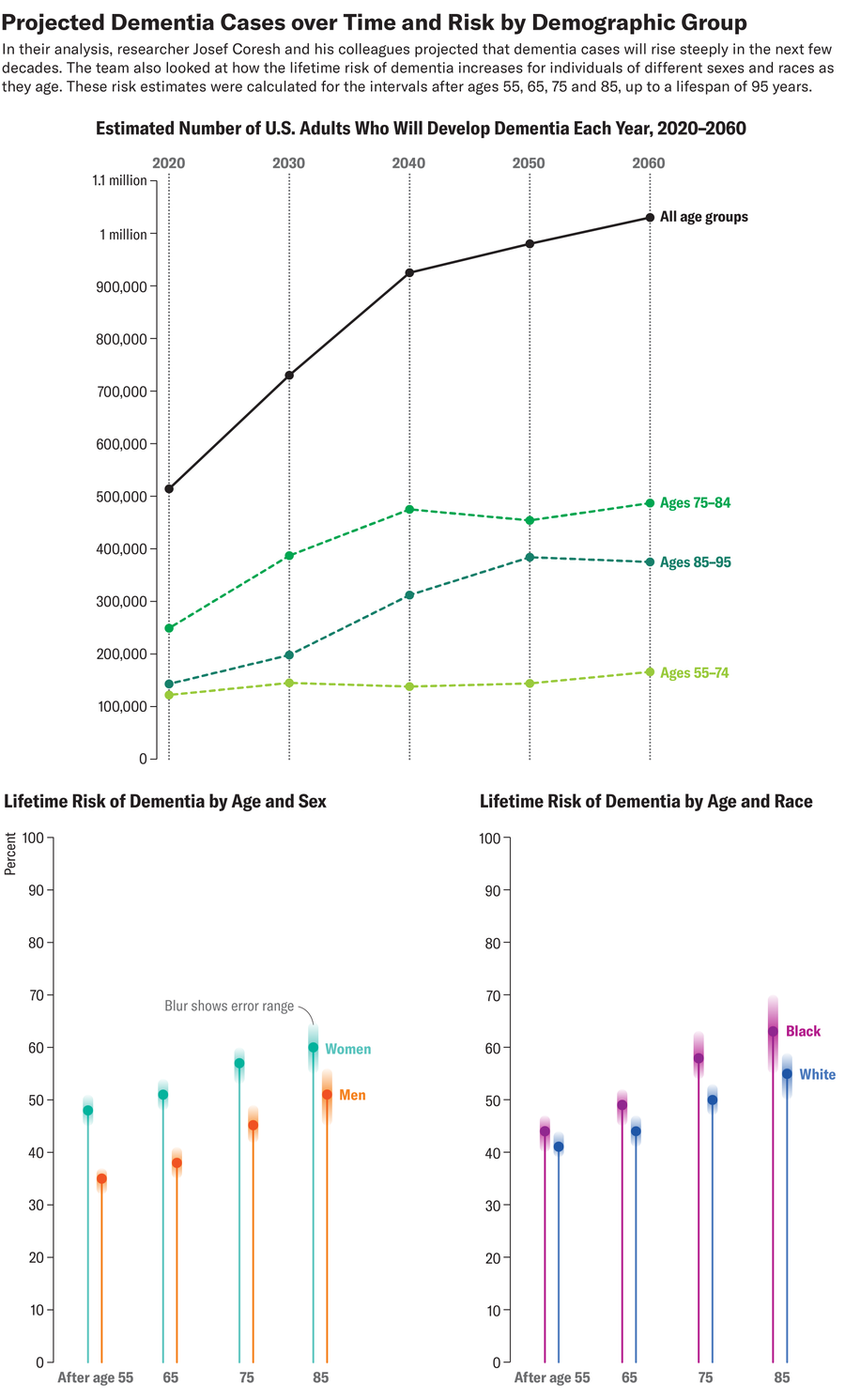
In the new study, the researchers reported 3,252 dementia cases and found the likelihood of developing dementia by age 95 after age 55 was 42 percent. Women’s lifetime risk was projected to be greater after age 55, at 48 percent, compared with 35 percent in men. After age 55, adults with two copies of APOE e4 had a higher lifetime risk (59 percent) than people with only one copy (48 percent). At that age, those with no copies of the allele had a 39 percent lifetime risk. The team then used U.S. Census Bureau projections to estimate the annual number of dementia cases from 2020 to 2060.
Coresh says the U.S.’s growing population of aging people is likely the primary driver behind the new study’s projected increase in dementia rates. “You can see how steep [the risk grows] with age, especially as the population over age 85 increases dramatically,” he says. The current average U.S. lifespan is about 75 years in men and 80 in women, although recent research suggests that from 2022 to 2050, global life expectancy will increase by approximately five years.
Nancy McLinskey, a neurologist at Stony Brook Medicine, who was not involved with the new study, says the results are not too surprising, considering the large number of older patients entering her clinic who require dementia care. “As the population lives longer, we’re going to see a significant increase in cases,” she says.
The study’s projected rise in dementia cases varied by race. Yearly dementia cases are set to alarmingly double among white adults. And cases among Black adults are even more staggering: their risk is expected to triple.
Black Americans often have higher rates of heart disease, which some studies suggest could be a risk factor for dementia. Additionally, Black people disproportionately experience medical racism, often resulting in late diagnoses and the lack of dementia treatments. McLinskey says the new report’s greater inclusion of Black participants compared with past studies could reflect a “potentially more accurate” picture of rising dementia rates.
While the study’s findings are consistent with some recent models, other data show different trajectories. A 2024 Alzheimer’s Association report states that Alzheimer’s and other types of dementia in the U.S. and other high-income countries may have actually declined in the past 25 years.
McLinskey says this decline could come from the development of better treatments for dementia risk factors, such as high blood pressure and diabetes (both of which can increase the risk of brain blood vessel damage). Greater access to continued education for older adults may also promote learning, which helps people withstand age- and disease-related brain changes.
Spurred by an increase in life expectancy and a decline in birth rates, the rapid growth of the country’s aging population could potentially thwart current improvements, Coresh says. He emphasizes the need for people to take preventative action now—even for those who are already older than age 55. “Dementia risk is high at older ages,” he says, “but a good amount of it is still preventable with better vascular health.”

